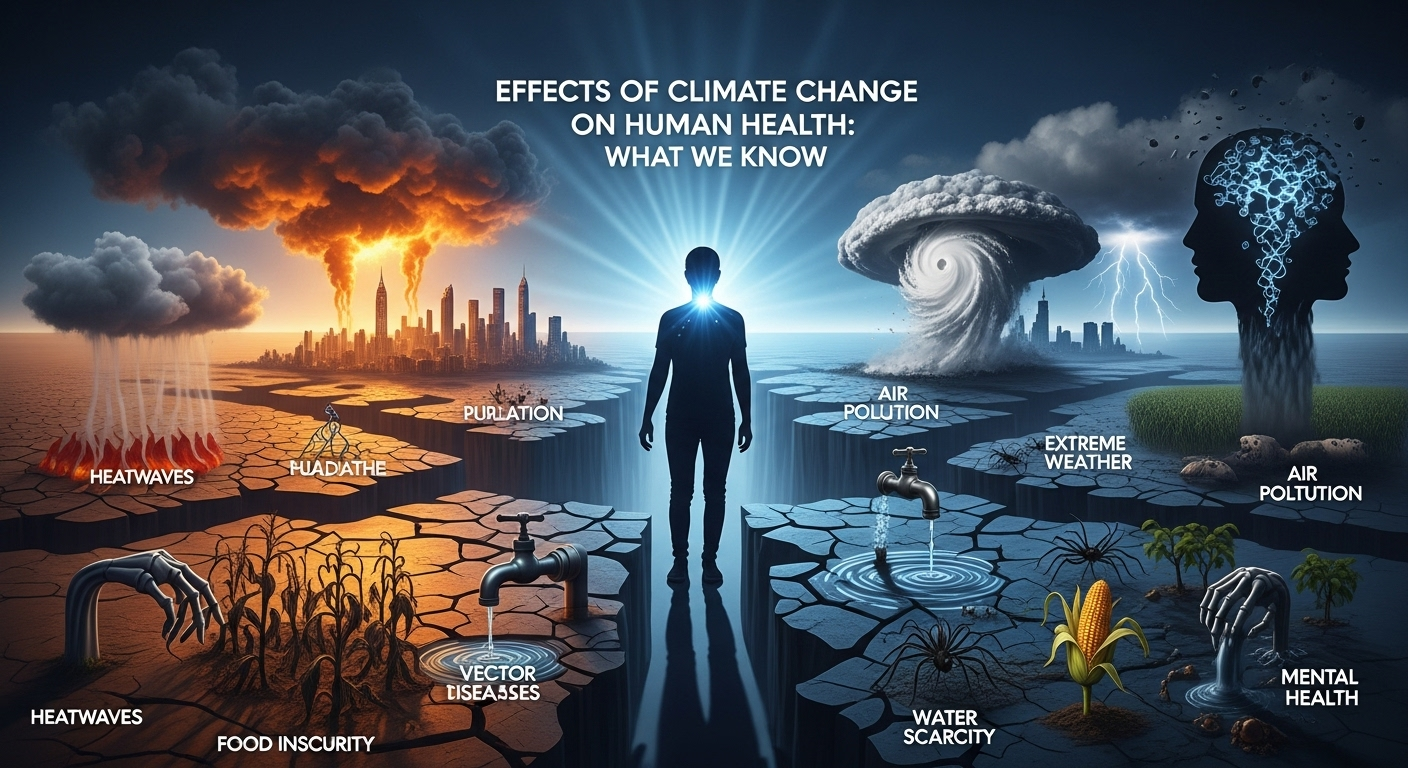
Effects of climate change on human health are already being observed around the world, from rising heat-related deaths to expanding ranges of infectious diseases. This article reviews the latest evidence on how changing climate patterns affect human wellbeing, healthcare systems, and communities—and it highlights practical responses policymakers, clinicians, and individuals can pursue to reduce harm and build resilience. H2: Heat, Extreme Weather, and Direct Health Impacts Extreme heat and more frequent heatwaves are among the clearest ways the climate crisis affects human bodies and health systems. Rising temperatures increase the risk of heat exhaustion, heatstroke, and worsening outcomes for people with cardiovascular and respiratory disease. Heat waves can also strain healthcare infrastructure, reduce labor productivity, and increase mortality rates, especially when nighttime temperatures remain high and prevent physiological recovery. Heat-related Illnesses Heat exposure triggers a range of clinical conditions from mild heat cramps and syncope to life‑threatening heatstroke. Elderly people, outdoor workers, infants, and those with chronic illnesses are particularly vulnerable. In urban areas, the urban heat island effect amplifies temperature increases, and areas with limited green space face disproportionate risk. Heat stress also interacts with other health conditions. For example, dehydration and electrolyte imbalances can worsen kidney disease; higher temperatures can increase the metabolic demands on people with heart disease; and some medications interfere with thermoregulation. Early warning systems, community cooling centers, and workplace protections are essential public health tools. Extreme Weather Events Storms, floods, hurricanes, and wildfires have immediate health consequences—injuries, traumatic deaths, and acute exacerbation of chronic illnesses—and longer-term effects from displacement and infrastructure disruption. Flooded hospitals, contaminated water supplies, and interrupted electricity can compromise care for people on dialysis or reliant on medical devices. Repeated or sequential disasters increase cumulative harm. Communities hit by one extreme event before they recover from the prior event face compounded mental health burdens and loss of social capital. Improving infrastructure resilience and integrating disaster preparedness into health systems reduces both immediate and prolonged harms. H2: Air Quality, Wildfires, and Cardiorespiratory Health Air pollution and climate-driven wildfire smoke are key mediators of health impacts. Warmer and drier conditions lengthen wildfire seasons and increase the frequency of large fires, which release fine particulate matter (PM2.5) and toxic gases that travel thousands of kilometers. Poor air quality aggravates asthma, COPD, cardiovascular disease, and is linked to increased mortality. Wildfire Smoke and Particulate Matter Wildfire smoke contains PM2.5, carbon monoxide, and volatile organic compounds that penetrate deep into the lungs and bloodstream. Short-term exposure increases emergency department visits for respiratory and cardiac events; long-term or repeated exposures are linked to chronic heart and lung disease. Air quality advisories, high-efficiency filtration indoors, and public guidance for evacuation or mask use are critical mitigation measures. Vulnerable groups—children, older adults, pregnant people, and those with pre-existing respiratory or cardiovascular illness—bear disproportionate burdens. Investing in forest management combined with emissions reduction strategies lowers both fire risk and population exposure. Ozone, Pollutants, and Heart Disease Rising temperatures enhance ground-level ozone formation, worsening smog and respiratory inflammation. Ozone and other pollutants also elevate the risk of hypertension, arrhythmias, and ischemic events. The combined burden of heat and poor air quality can overwhelm emergency services during heatwaves and wildfire episodes. Public health messaging should integrate air quality, heat advisories, and guidance on safe outdoor activity. Urban planning that reduces vehicle emissions and increases green infrastructure can produce co-benefits—improved air, lower temperatures, and better public health. H2: Infectious Diseases, Vectors, and Waterborne Illnesses Climate change alters ecosystems, vector distributions, and water systems—shifting the epidemiology of many infectious diseases. Warmer temperatures, changing precipitation patterns, and extreme events can expand the geographic range and seasonality of vector-borne diseases (mosquitoes, ticks), increase waterborne outbreaks, and complicate food safety. Vector Range Shifts Mosquitoes that transmit dengue, chikungunya, Zika, and malaria are sensitive to temperature and humidity. As climates warm, some species expand into higher altitudes and latitudes, exposing new populations to disease. Tick-borne illnesses such as Lyme disease are also shifting, with longer transmission seasons and increased case counts in some regions. Surveillance, vector control, vaccines where available, and public awareness campaigns are essential. Health systems must adapt laboratory and clinical capacity to recognize diseases that were previously rare in certain areas. Integrated vector management that combines environmental controls, community engagement, and targeted insecticide use can reduce transmission risk. Waterborne and Foodborne Diseases Heavy rainfall and floods can contaminate drinking water with pathogens (e.g., cholera, norovirus) and increase the risk of gastrointestinal outbreaks. Conversely, droughts can concentrate pathogens and pollutants in limited water supplies. Rising temperatures may also favor growth of harmful algal blooms and foodborne pathogens like Salmonella, increasing illness risk. Strengthening water and sanitation infrastructure, ensuring access to safe drinking water, and rapid detection systems are critical. Climate-smart agricultural practices and cold-chain resilience reduce food safety risks, while community education on hygiene and safe food handling mitigates immediate exposures. H2: Mental Health, Displacement, and Social Determinants Health impacts of climate change are not only physical; they deeply affect mental health, social stability, and the determinants of health such as housing, income, and access to care. Chronic stress, grief over environmental loss, and trauma from disasters contribute to rising rates of depression, anxiety, and post-traumatic stress disorder (PTSD). Climate Anxiety and PTSD Younger generations frequently report climate anxiety—a persistent worry about future climate harms. Acute events like hurricanes or wildfire evacuations can produce PTSD, while slow-onset changes (sea-level rise, loss of livelihoods) can erode mental wellbeing over time. Mental health services often lack capacity or funding to manage these growing needs. Community-based interventions, culturally appropriate counseling, and integration of mental health into disaster response improve outcomes. Building social cohesion and restoring local environments (e.g., community greening) can provide therapeutic benefits and strengthen resilience. Migration, Displacement, and Health Services Climate-related displacement—temporary or permanent—creates complex health challenges. Displaced populations may face overcrowded shelters, interrupted care for chronic diseases, increased exposure to infectious diseases, and barriers to mental healthcare. Host communities can experience strain on services and social tensions. Planning for managed retreat, improving shelter standards, and